One Mark Question and Answer
- What is the primary purpose of oxygen utilization in living cells?
Ans: Oxygen is utilized to indirectly break down simple molecules like glucose to derive energy for various activities.
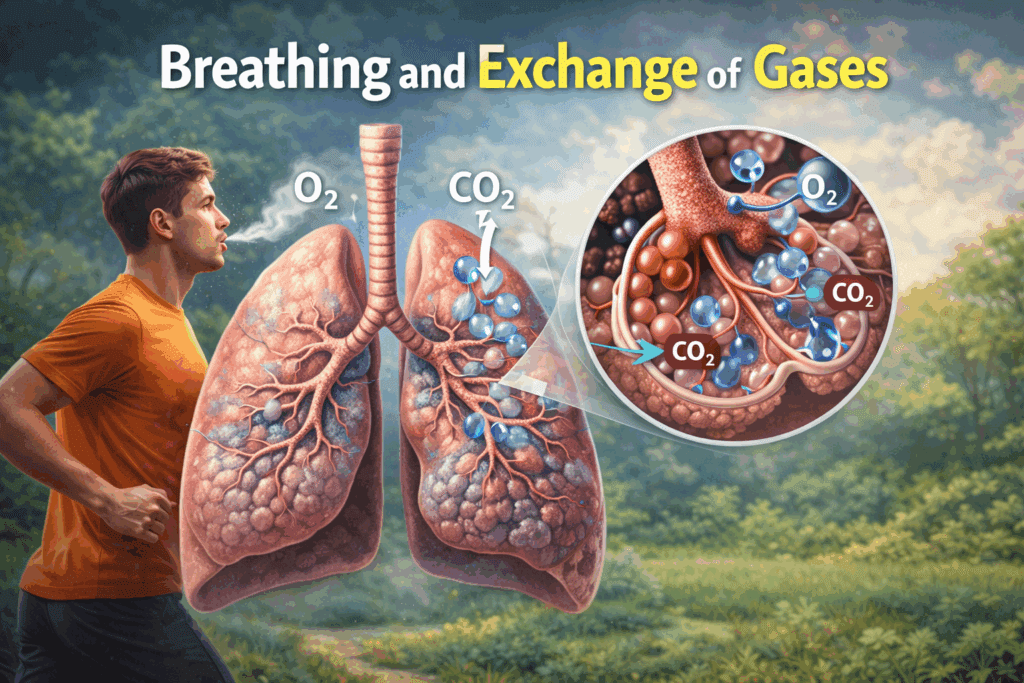
- Define breathing.
Ans: Breathing is the process of exchange of oxygen from the atmosphere with carbon dioxide produced by the cells.
- Name the mechanism of gas exchange used by lower invertebrates like sponges.
Ans: They exchange gases by simple diffusion over their entire body surface.
- Which respiratory structure is used by earthworms for gas exchange?
Ans: Earthworms use their moist cuticle for respiration.
- How do insects transport atmospheric air within their bodies?
Ans: Insects have a network of tubes called tracheal tubes to transport air.
- What is branchial respiration?
Ans: It is respiration mediated by special vascularised structures called gills, common in aquatic arthropods and molluscs.
- What is pulmonary respiration?
Ans: Pulmonary respiration is the exchange of gases using vascularised bags called lungs, used by terrestrial forms.
- Name the group of vertebrates that respire mainly through gills.
Ans: Fishes respire mainly through gills.
- Besides lungs, how can amphibians like frogs respire?
Ans: Frogs can respire through their moist skin, known as cutaneous respiration.
- Why must carbon dioxide be released from the cells?
Ans: Carbon dioxide is released because it is a harmful by-product of catabolic reactions.
- Trace the path of air from the nostrils to the pharynx.
Ans: External nostrils lead to a nasal chamber through the nasal passage, which then opens into the pharynx.
- What is the common passage for both food and air in the human body?
Ans: The pharynx is the common passage for food and air.
- What is the function of the epiglottis?
Ans: The epiglottis is a flap that covers the glottis during swallowing to prevent food from entering the larynx.
- Why is the larynx known as the sound box?
Ans: The larynx is a cartilaginous box that helps in sound production.
- Describe the structure of the trachea.
Ans: The trachea is a straight tube extending to the mid-thoracic cavity supported by incomplete cartilaginous rings.
- At which anatomical level does the trachea divide?
Ans: The trachea divides at the level of the 5th thoracic vertebra.
- Into what structures does the trachea divide?
Ans: It divides into a right and left primary bronchi.
- What supports the primary, secondary, and tertiary bronchi to prevent collapse?
Ans: They are supported by incomplete cartilaginous rings.
- What are terminal bronchioles?
Ans: They are very thin tubes that result from the repeated division of bronchi and bronchioles.
- Identify the structure diagrammatically located below the lungs that aids in breathing.
Ans: The diaphragm.
- Define alveoli.
Ans: Alveoli are very thin, irregular-walled, and vascularised bag-like structures where gas exchange occurs.
- What constitutes the lungs?
Ans: The branching network of bronchi, bronchioles, and alveoli comprise the lungs.
- What is the function of the pleural fluid?
Ans: Pleural fluid reduces friction on the lung surface.
- Name the double-layered membrane covering the lungs.
Ans: The pleura (or pleural membranes).
- Differentiate between the outer and inner pleural membranes regarding their contact.
Ans: The outer membrane is in contact with the thoracic lining, while the inner membrane is in contact with the lung surface.
- What constitutes the conducting part of the respiratory system?
Ans: The part starting from the external nostrils up to the terminal bronchioles.
- State one function of the conducting part of the respiratory system.
Ans: It clears atmospheric air from foreign particles, humidifies it, and brings it to body temperature.
- What defines the exchange part of the respiratory system?
Ans: The alveoli and their ducts form the exchange part, where diffusion of O2 and CO2 takes place.
- Describe the dorsal boundary of the thoracic chamber.
Ans: The thoracic chamber is formed dorsally by the vertebral column.
- Why is the air-tight setup of the thoracic chamber essential?
Ans: It is essential because we cannot directly alter the pulmonary volume; changes in thoracic volume are required to change pulmonary volume for breathing.
- What is the first step of respiration?
Ans: Breathing or pulmonary ventilation, where atmospheric air is drawn in and alveolar air is released.
- What pressure condition is required for inspiration to occur?
Ans: Inspiration occurs if the intra-pulmonary pressure is less than the atmospheric pressure (negative pressure).
- When does expiration take place regarding pressure gradients?
Ans: Expiration takes place when the intra-pulmonary pressure is higher than the atmospheric pressure.
- Which muscles are primarily responsible for generating pressure gradients for breathing?
Ans: The diaphragm and the external and internal intercostal muscles.
- How does the diaphragm aid in inspiration?
Ans: The contraction of the diaphragm increases the volume of the thoracic chamber in the antero-posterior axis.
- What is the role of external inter-costal muscles during inspiration?
Ans: Their contraction lifts the ribs and sternum, increasing thoracic chamber volume in the dorso-ventral axis.
- What is the relationship between thoracic volume and pulmonary volume?
Ans: An overall increase in thoracic volume causes a similar increase in pulmonary volume.
- How does an increase in pulmonary volume affect intra-pulmonary pressure?
Ans: It decreases the intra-pulmonary pressure to less than the atmospheric pressure, causing inspiration.
- What movement defines the initiation of expiration?
Ans: The relaxation of the diaphragm and inter-costal muscles returning the sternum to its normal position.
- Define intra-pulmonary pressure.
Ans: It is the pressure within the lungs.
- How can humans increase the strength of inspiration and expiration?
Ans: By using additional muscles in the abdomen.
- What is the average breathing rate of a healthy human? Ans: A healthy human breathes 12–16 times per minute.
- What is the clinical utility of a spirometer?
Ans: It helps in the clinical assessment of pulmonary functions by estimating the volume of air involved in breathing.
- Define Tidal Volume (TV).
Ans: TV is the volume of air inspired or expired during normal respiration, approximately 500 mL.
- What is Inspiratory Reserve Volume (IRV)?
Ans: It is the additional volume of air a person can inspire by a forcible inspiration (2500 mL to 3000 mL).
- Define Expiratory Reserve Volume (ERV).
Ans: It is the additional volume of air a person can expire by a forcible expiration (1000 mL to 1100 mL).
- Define Residual Volume (RV).
Ans: RV is the volume of air remaining in the lungs even after a forcible expiration (1100 mL to 1200 mL).
- Can Residual Volume be measured directly by a spirometer?
Ans: No, because it is the air remaining in lungs after forceful expiration (Note: This is an inference based on the definition of RV and spirometry mechanics).
- Calculate the volume of air a healthy man can inspire per minute.
Ans: Approximately 6000 to 8000 mL per minute.
- What constitutes the Inspiratory Capacity (IC)?
Ans: IC is the total volume of air a person can inspire after a normal expiration (TV + IRV).
- Define Functional Residual Capacity (FRC).
Ans: FRC is the volume of air remaining in the lungs after a normal expiration (ERV + RV).
- What represents Vital Capacity (VC)?
Ans: The maximum volume of air a person can breathe in after a forced expiration (ERV + TV + IRV).
- Define Total Lung Capacity (TLC).
Ans: TLC is the total volume of air accommodated in the lungs at the end of a forced inspiration (VC + RV).
- What is the primary site of exchange of gases?
Ans: The alveoli are the primary sites of exchange of gases.
- List two factors that affect the rate of gas diffusion.
Ans: Solubility of the gases and the thickness of the membranes involved in diffusion.
- Define partial pressure.
Ans: Pressure contributed by an individual gas in a mixture of gases.
- What is the partial pressure of Oxygen (pO2) in oxygenated blood?
Ans: 95 mm Hg.
- What is the partial pressure of CO2 in tissues?
Ans: 45 mm Hg.
- Compare the solubility of CO2 and O2.
Ans: The solubility of CO2 is 20-25 times higher than that of O2.
- What drives the diffusion of gases between blood and tissues?
Ans: Simple diffusion mainly based on pressure/concentration gradients.
- Name the three layers of the diffusion membrane.
Ans: The thin squamous epithelium of alveoli, the endothelium of alveolar capillaries, and the basement substance between them.
- What is the total thickness of the diffusion membrane?
Ans: Its total thickness is much less than a millimetre.
- In what form is the majority of oxygen transported in the blood?
Ans: About 97% of O2 is transported by RBCs as oxyhaemoglobin.
- How is the remaining 3% of oxygen transported?
Ans: It is carried in a dissolved state through the plasma.
- In what form is the majority (70%) of CO2 transported?
Ans: It is carried as bicarbonate.
- What is the maximum number of oxygen molecules a single haemoglobin molecule can carry?
Ans: Four molecules of O2.
- What type of curve is the Oxygen dissociation curve?
Ans: It is a sigmoid curve.
- List two factors in tissues that favor the dissociation of oxygen from oxyhaemoglobin.
Ans: Low pO2, high pCO2, high H+ concentration, or higher temperature.
- Where does O2 bind to haemoglobin to form oxyhaemoglobin?
Ans: In the lung surface (alveoli) where pO2 is high.
- How much oxygen is delivered to tissues by 100 ml of oxygenated blood under normal conditions?
Ans: Around 5 ml of O2.
- Name the compound formed when CO2 binds to haemoglobin. Ans: Carbamino-haemoglobin.
- What primary factor affects the binding of CO2 to haemoglobin?
Ans: The partial pressure of CO2 (pCO2).
- Name the enzyme in RBCs that facilitates CO2 transport.
Ans: Carbonic anhydrase.
- Write the reaction catalyzed by carbonic anhydrase.
Ans: CO2 + H2O ⇄ H2CO3 ⇄ HCO3– + H+.
- How much CO2 is delivered to the alveoli by 100 ml of deoxygenated blood?
Ans: Approximately 4 ml of CO2.
- Which center in the brain is primarily responsible for respiratory rhythm regulation?
Ans: The respiratory rhythm centre in the medulla region.
- Where is the pneumotaxic centre located?
Ans: In the pons region of the brain.
- What is the function of the pneumotaxic centre?
Ans: It can moderate the functions of the rhythm centre, specifically reducing the duration of inspiration.
- Which substances activate the chemosensitive area adjacent to the rhythm centre?
Ans: CO2 and hydrogen ions (H+).
- What is the role of oxygen in regulating respiratory rhythm?
Ans: The role of oxygen in the regulation of respiratory rhythm is quite insignificant.
- What characterizes Asthma?
Ans: Asthma is characterized by difficulty in breathing causing wheezing due to inflammation of bronchi and bronchioles.
- Define Emphysema.
Ans: It is a chronic disorder where alveolar walls are damaged, decreasing the respiratory surface.
- What is a major cause of Emphysema? Ans: Cigarette smoking is a major cause.
- What triggers Occupational Respiratory Disorders?
Ans: Long exposure to dust produced in industries like grinding or stone-breaking.
- What is fibrosis in the context of lung disorders?
Ans: Fibrosis is the proliferation of fibrous tissues causing serious lung damage.
- How should workers in dust-generating industries protect themselves?
Ans: They should wear protective masks.
- Summarize the first step of respiration.
Ans: Breathing, where atmospheric air is taken in (inspiration) and alveolar air is released out (expiration).
- How is 70% of carbon dioxide transported?
Ans: It is transported as bicarbonate (HCO3-) with the help of the enzyme carbonic anhydrase.
- Where does the dissociation of oxyhaemoglobin primarily occur?
Ans: It occurs at the tissues where pO2 is low and pCO2 is high.
- What happens to the pCO2 and pO2 in the alveoli to facilitate CO2 removal?
Ans: In the alveoli, pCO2 is low and pO2 is high, causing CO2 to be removed from the blood.
Two Mark Question and Answer
Q1: Why is the continuous supply of oxygen to cells essential for survival?
Ans: Oxygen is utilized by organisms to indirectly break down simple molecules like glucose and fatty acids to derive energy for various activities. Additionally, this process is necessary to facilitate the release of carbon dioxide, which is a harmful by-product of catabolic reactions.
Q2: Define breathing and distinguish it from the broader concept of respiration.
Ans: Breathing is the specific process of exchanging oxygen from the atmosphere with carbon dioxide produced by the cells. It is commonly referred to as respiration, though respiration also encompasses the cellular utilisation of oxygen for energy production.
Q3: Describe the mechanism of gas exchange in lower invertebrates like sponges and flatworms.
Ans: Lower invertebrates such as sponges, coelenterates, and flatworms do not have specialized respiratory organs. They exchange oxygen and carbon dioxide by simple diffusion over their entire body surface.
Q4: How do earthworms perform respiration?
Ans: Earthworms lack distinct respiratory organs and instead use their moist cuticle. Gas exchange occurs directly through this moist surface.
Q5: What are tracheal tubes and which group of animals primarily uses them?
Ans: Tracheal tubes are a network of tubes used to transport atmospheric air within the body. These are primarily found in insects.
Q6: Differentiate between branchial and pulmonary respiration.
Ans: Branchial respiration involves the use of special vascularised structures called gills, common in aquatic arthropods and molluscs. Pulmonary respiration involves vascularised bags called lungs, used by terrestrial forms for gas exchange.
Q7: Which vertebrate groups respire primarily through lungs?
Ans: Among vertebrates, reptiles, birds, and mammals respire through lungs. Amphibians also respire through lungs, although they have alternative methods as well.
Q8: Explain how amphibians like frogs exhibit a dual mode of respiration.
Ans: Amphibians like frogs respire through lungs (pulmonary respiration). However, they can also respire through their moist skin, a process known as cutaneous respiration.
Q9: What dictates the mechanism of breathing in different animal groups?
Ans: The mechanism of breathing varies among different groups of animals depending mainly on their habitats and their levels of organisation.
Q10: What are the two main requirements for the catabolic reactions in cells mentioned in the text?
Ans: The two main requirements are the continuous provision of oxygen to the cells and the release/removal of carbon dioxide produced by the cells.
Q11: Describe the path of air from the external nostrils to the pharynx.
Ans: Air enters through a pair of external nostrils located above the upper lips. It then passes through the nasal passage into the nasal chamber, which opens into the pharynx.
Q12: What is the pharynx and what is its unique functional characteristic?
Ans: The pharynx is a portion of the respiratory tract into which the nasal chamber opens. It serves as a common passage for both food and air.
Q13: Explain the role of the epiglottis during swallowing.
Ans: The epiglottis is a thin, elastic cartilaginous flap. During swallowing, it covers the glottis to prevent the entry of food into the larynx.
Q14: Why is the larynx referred to as the “sound box”?
Ans: The larynx is a cartilaginous box located at the top of the trachea. It helps in sound production, earning it the name “sound box”.
Q15: Describe the anatomical structure and location of the trachea.
Ans: The trachea is a straight tube that extends up to the mid-thoracic cavity. It is supported by incomplete cartilaginous rings to prevent collapse.
Q16: At what anatomical level does the trachea divide, and what does it divide into?
Ans: The trachea divides at the level of the 5th thoracic vertebra. It divides into a right and a left primary bronchi.
Q17: Describe the branching hierarchy of the bronchial tree.
Ans: Each primary bronchus undergoes repeated divisions to form secondary and tertiary bronchi. These further divide into bronchioles, eventually ending in very thin terminal bronchioles.
Q18: Which parts of the respiratory tract are supported by cartilaginous rings?
Ans: The trachea, primary bronchi, secondary bronchi, tertiary bronchi, and the initial bronchioles are supported by incomplete cartilaginous rings.
Q19: What are alveoli and where do they originate?
Ans: Alveoli are very thin, irregular-walled, and vascularised bag-like structures. They arise from the terminal bronchioles.
Q20: What structures collectively comprise the lungs?
Ans: The branching network of bronchi, bronchioles, and alveoli collectively comprise the lungs.
Q21: Describe the pleural membranes and their orientation.
Ans: The lungs are covered by a double-layered pleura. The outer pleural membrane is in close contact with the thoracic lining, while the inner pleural membrane is in contact with the lung surface.
Q22: What is the function of the pleural fluid?
Ans: Pleural fluid is located between the two layers of the pleura. Its primary function is to reduce friction on the lung surface during breathing movements.
Q23: Define the “conducting part” of the respiratory system and list its components.
Ans: The conducting part starts from the external nostrils and extends up to the terminal bronchioles. It includes the nostrils, nasal chamber, pharynx, larynx, trachea, bronchi, and bronchioles.
Q24: What are the specific functions of the conducting part of the respiratory system?
Ans: The conducting part transports atmospheric air to the alveoli, clears it of foreign particles, humidifies it, and brings the air to body temperature.
Q25: Define the “exchange part” of the respiratory system and state its function.
Ans: The exchange part consists of the alveoli and their ducts. It is the site of the actual diffusion of oxygen and carbon dioxide between the blood and atmospheric air.
Q26: Describe the dorsal and ventral boundaries of the thoracic chamber.
Ans: The thoracic chamber is formed dorsally by the vertebral column and ventrally by the sternum.
Q27: Describe the lateral and lower boundaries of the thoracic chamber.
Ans: Laterally, the thoracic chamber is formed by the ribs. On the lower side, it is formed by the dome-shaped diaphragm.
Q28: Why is the thoracic chamber described as “anatomically air-tight”?
Ans: It is a closed cavity formed by bones and muscles (vertebrae, sternum, ribs, diaphragm) with no direct opening to the outside except through the trachea. This setup ensures that volume changes in the thorax are directly reflected in the lungs.
Q29: Explain the physiological significance of the anatomical setup of the lungs in the thorax.
Ans: The setup ensures that any change in the volume of the thoracic cavity is reflected in the pulmonary cavity. This is essential because humans cannot directly alter pulmonary volume; they must manipulate thoracic volume to breathe.
Q30: List the first two steps of respiration.
Ans: The first step is breathing (pulmonary ventilation) where atmospheric air is drawn in and alveolar air is released. The second step is the diffusion of gases (O2 and CO2) across the alveolar membrane.
Q31: What are the third, fourth, and fifth steps of respiration? Ans: (iii) Transport of gases by the blood; (iv) Diffusion of O2 and CO2 between blood and tissues; (v) Utilisation of O2 by cells for catabolic reactions and release of CO2.
Q32: What creates the movement of air into and out of the lungs?
Ans: The movement is carried out by creating a pressure gradient between the lungs and the atmosphere. Air moves from areas of high pressure to areas of low pressure.
Q33: Define the conditions required for inspiration to occur.
Ans: Inspiration occurs when the intra-pulmonary pressure (pressure within the lungs) is less than the atmospheric pressure. This creates a negative pressure in the lungs relative to the atmosphere.
Q34: Define the conditions required for expiration to occur.
Ans: Expiration takes place when the intra-pulmonary pressure is higher than the atmospheric pressure, forcing air out of the lungs.
Q35: Which specific muscle groups are responsible for generating pressure gradients for breathing?
Ans: The diaphragm and a specialised set of muscles known as the external and internal intercostals (located between the ribs) are responsible.
Q36: Explain the mechanism of inspiration involving the diaphragm.
Ans: Inspiration is initiated by the contraction of the diaphragm. This contraction flattens the diaphragm, increasing the volume of the thoracic chamber in the antero-posterior axis.
Q37: Explain the role of external intercostal muscles in inspiration.
Ans: The contraction of external inter-costal muscles lifts up the ribs and the sternum. This action increases the volume of the thoracic chamber in the dorso-ventral axis.
Q38: How does an increase in thoracic volume lead to inspiration?
Ans: An increase in thoracic volume causes a similar increase in pulmonary volume. This increase reduces the intra-pulmonary pressure to below atmospheric pressure, forcing outside air into the lungs.
Q39: Describe the mechanism of relaxation that leads to expiration.
Ans: Relaxation of the diaphragm and inter-costal muscles returns the diaphragm and sternum to their normal positions. This reduces thoracic and pulmonary volume, increasing intra-pulmonary pressure and expelling air.
Q40: What is the difference between intra-pulmonary pressure during inspiration and expiration relative to atmospheric pressure?
Ans: During inspiration, intra-pulmonary pressure is lower (negative) than atmospheric pressure. During expiration, intra-pulmonary pressure is slightly higher than atmospheric pressure.
Q41: How can the strength of inspiration and expiration be increased beyond normal breathing?
Ans: Humans can increase the strength of inspiration and expiration by utilizing additional muscles located in the abdomen.
Q42: What is the average breathing rate of a healthy human and how is it measured clinically?
Ans: A healthy human breathes 12–16 times per minute. The volume of air involved can be estimated using a spirometer for clinical assessment.
Q43: Define Tidal Volume (TV) and provide its approximate volume per minute.
Ans: Tidal Volume is the volume of air inspired or expired during normal respiration (approx. 500 mL). Per minute, a healthy man can inspire or expire 6000 to 8000 mL of air.
Q44: Define Inspiratory Reserve Volume (IRV) and state its average range.
Ans: IRV is the additional volume of air a person can inspire by a forcible inspiration. It averages between 2500 mL and 3000 mL.
Q45: Define Expiratory Reserve Volume (ERV) and state its average range.
Ans: ERV is the additional volume of air a person can expire by a forcible expiration. It averages between 1000 mL and 1100 mL.
Q46: Define Residual Volume (RV) and explain why it exists.
Ans: Residual Volume is the volume of air remaining in the lungs even after a forcible expiration. It exists because the lungs never completely collapse; this volume averages 1100 mL to 1200 mL.
Q47: Can a spirometer measure all respiratory volumes? Explain.
Ans: No, a spirometer measures air inspired or expired. Therefore, it cannot measure the Residual Volume (RV), as this air cannot be exhaled.
Q48: Differentiate between TV and ERV.
Ans: TV (500 mL) is the air moved during normal breathing. ERV (1000-1100 mL) is the additional air that can be forcibly exhaled after a normal expiration.
Q49: Calculate the total volume of air inspired in 5 minutes by a healthy person (using average TV).
Ans: With an average TV of 500 mL and a breathing rate of 12-16 times/min, the minute volume is 6000-8000 mL. In 5 minutes, this would be approximately 30,000 to 40,000 mL.
Q50: Arrange TV, ERV, IRV, and RV in ascending order of their average volumes.
Ans: TV (500 mL) < ERV (1000-1100 mL) < RV (1100-1200 mL) < IRV (2500-3000 mL).
Q51: Define Inspiratory Capacity (IC) and give its formula.
Ans: IC is the total volume of air a person can inspire after a normal expiration. It is calculated as Tidal Volume plus Inspiratory Reserve Volume (TV + IRV).
Q52: Define Expiratory Capacity (EC) and give its formula.
Ans: EC is the total volume of air a person can expire after a normal inspiration. It is calculated as Tidal Volume plus Expiratory Reserve Volume (TV + ERV).
Q53: What is Functional Residual Capacity (FRC)?
Ans: FRC is the volume of air that remains in the lungs after a normal expiration. It includes Expiratory Reserve Volume and Residual Volume (ERV + RV).
Q54: Define Vital Capacity (VC).
Ans: VC is the maximum volume of air a person can breathe in after a forced expiration (or breathe out after a forced inspiration). It includes ERV, TV, and IRV.
Q55: What is Total Lung Capacity (TLC)?
Ans: TLC is the total volume of air accommodated in the lungs at the end of a forced inspiration. It is the sum of Vital Capacity and Residual Volume (VC + RV) or (RV + ERV + TV + IRV).
Q56: Identify the primary sites for gas exchange in the human body.
Ans: The alveoli are the primary sites of exchange of gases. Exchange also occurs between blood and tissues.
Q57: What is the physical basis for the exchange of gases in the alveoli?
Ans: Gases (O2 and CO2) are exchanged by simple diffusion. This is driven mainly by the pressure or concentration gradient of the gases.
Q58: Apart from pressure gradients, what two factors influence the rate of diffusion?
Ans: The solubility of the gases and the thickness of the membranes involved in diffusion are important factors affecting the rate.
Q59: Define Partial Pressure and its symbol.
Ans: Partial pressure is the pressure contributed by an individual gas in a mixture of gases. It is represented as pO2 for oxygen and pCO2 for carbon dioxide.
Q60: Using the data from the text, compare the pO2 in the alveoli vs. the tissues.
Ans: The pO2 in the alveoli is high (104 mm Hg), whereas the pO2 in the tissues is low (40 mm Hg). This creates a gradient for oxygen diffusion from alveoli to tissues.
Q61: Compare the solubility of CO2 and O2 and explain its significance in diffusion.
Ans: The solubility of CO2 is 20-25 times higher than that of O2. Consequently, the amount of CO2 that can diffuse through the membrane per unit partial pressure difference is much higher than that of O2.
Q62: Name the three layers that constitute the diffusion membrane.
Ans: The layers are the thin squamous epithelium of the alveoli, the endothelium of alveolar capillaries, and the basement substance in between them.
Q63: Comment on the thickness of the diffusion membrane and its impact on gas exchange.
Ans: The total thickness of the diffusion membrane is much less than a millimetre. This thinness creates a favorable condition for the rapid diffusion of O2 and CO2.
Q64: Describe the gradient for CO2 transport.
Ans: A partial pressure gradient for CO2 exists in the opposite direction to O2. It is higher in the tissues (45 mm Hg) and lower in the alveoli (40 mm Hg), facilitating removal.
Q65: In what two forms is oxygen transported in the blood?
Ans: About 97% of oxygen is transported by RBCs (as oxyhaemoglobin). The remaining 3% is carried in a dissolved state through the plasma.
Q66: In what three forms is carbon dioxide transported in the blood?
Ans: Nearly 20-25% is transported by RBCs (carbamino-haemoglobin), 70% is carried as bicarbonate, and about 7% is dissolved in plasma.
Q67: What is haemoglobin and what is its capacity for oxygen binding?
Ans: Haemoglobin is a red-coloured iron-containing pigment in RBCs. Each haemoglobin molecule can carry a maximum of four molecules of O2.
Q68: What primary factor determines the binding of oxygen to haemoglobin?
Ans: The binding of oxygen with haemoglobin is primarily related to the partial pressure of O2 (pO2).
Q69: List three factors that can interfere with O2 binding to haemoglobin.
Ans: The partial pressure of CO2 (pCO2), hydrogen ion concentration (pH), and temperature can interfere with O2 binding.
Q70: Describe the Oxygen Dissociation Curve.
Ans: It is a sigmoid curve obtained when the percentage saturation of haemoglobin with O2 is plotted against pO2. It helps in studying the effect of factors like pCO2 and H+ concentration on binding.
Q71: Contrast the conditions in the alveoli vs. tissues regarding Oxyhaemoglobin formation.
Ans: In alveoli, high pO2, low pCO2, low H+, and low temperature favor oxyhaemoglobin formation. In tissues, low pO2, high pCO2, high H+, and high temperature favor dissociation.
Q72: What is the physiological output of oxygen delivery to tissues?
Ans: Every 100 ml of oxygenated blood can deliver around 5 ml of O2 to the tissues under normal physiological conditions.
Q73: How is CO2 transported by haemoglobin and what affects this binding?
Ans: CO2 is carried as carbamino-haemoglobin (20-25%). This binding is primarily related to pCO2, but pO2 is a major factor that affects it (high pO2 interferes with binding).
Q74: Explain the role of Carbonic Anhydrase in CO2 transport.
Ans: This enzyme, found in RBCs and plasma, facilitates the conversion of CO2 and H2O into carbonic acid (H2CO3) and subsequently into bicarbonate (HCO3-) and H+.
Q75: Describe the reaction of CO2 at the tissue level.
Ans: At the tissue site, where pCO2 is high due to catabolism, CO2 diffuses into the blood and reacts with water to form HCO3- (bicarbonate) and H+.
Q76: What happens to bicarbonate at the alveolar site?
Ans: At the alveolar site, where pCO2 is low, the reaction proceeds in the reverse direction, converting bicarbonate and H+ back into CO2 and H2O, allowing CO2 release.
Q77: How much CO2 is delivered to the lungs by blood?
Ans: Every 100 ml of deoxygenated blood delivers approximately 4 ml of CO2 to the alveoli.
Q78: Which part of the brain is primarily responsible for respiratory rhythm?
Ans: A specialised centre in the medulla region of the brain called the respiratory rhythm centre is primarily responsible for regulation.
Q79: What is the Pneumotaxic centre and what is its function?
Ans: It is a centre in the pons region of the brain. It moderates the rhythm centre, primarily by reducing the duration of inspiration to alter the respiratory rate.
Q80: How does the chemosensitive area regulate respiration?
Ans: Located adjacent to the rhythm centre, it is highly sensitive to CO2 and H+ ions. An increase in these substances activates the area, signaling the rhythm centre to increase respiration and eliminate them.
Q81: What is the role of the aortic arch and carotid artery receptors in respiratory regulation?
Ans: These receptors recognize changes in CO2 and H+ concentration in the blood. They send signals to the rhythm centre for remedial actions.
Q82: What is the significance of oxygen in the regulation of respiratory rhythm?
Ans: The role of oxygen in the regulation of respiratory rhythm is quite insignificant compared to CO2 and H+ ions.
Q83: Define Asthma and its primary symptoms.
Ans: Asthma is a respiratory disorder characterized by difficulty in breathing and wheezing. It is caused by the inflammation of the bronchi and bronchioles.
Q84: What is Emphysema and what is its major cause?
Ans: Emphysema is a chronic disorder where alveolar walls are damaged, decreasing the respiratory surface area. A major cause is cigarette smoking.
Q85: What characterizes Occupational Respiratory Disorders?
Ans: These disorders arise in industries (like grinding/stone-breaking) where dust production overwhelms the body’s defense mechanisms.
Q86: What is fibrosis and how is it related to occupational hazards?
Ans: Fibrosis is the proliferation of fibrous tissues. It occurs due to long-term exposure to industrial dust, leading to serious lung damage.
Q87: What preventative measure is suggested for workers in stone-breaking industries?
Ans: Workers in such industries are advised to wear protective masks to prevent dust inhalation.
Q88: Summarize the pressure conditions required for inspiration.
Ans: Inspiration occurs when intra-pulmonary pressure is lower than atmospheric pressure. This gradient allows air to flow into the lungs.
Q89: According to the summary, how is the majority of CO2 transported?
Ans: Nearly 70 percent of carbon dioxide is transported as bicarbonate (HCO3-) with the help of the enzyme carbonic anhydrase.
Q90: Summarize the factors favorable for the formation of Oxyhaemoglobin.
Ans: High pO2, low pCO2, and low H+ concentration (and lower temperature) in the alveoli are favorable for the binding of oxygen to haemoglobin.
Q91: Explain the primary physiological reason why cells require a continuous supply of oxygen.
Ans: Organisms utilize oxygen to indirectly break down simple molecules like glucose, amino acids, and fatty acids to derive energy for performing various activities. Furthermore, this process is essential to ensure the removal of carbon dioxide, which is a harmful by-product released during these catabolic reactions.
Q92: Differentiate between the respiratory organs of aquatic arthropods and terrestrial insects.
Ans: Aquatic arthropods typically use special vascularised structures called gills for respiration (branchial respiration). In contrast, terrestrial insects possess a network of tubes known as tracheal tubes to transport atmospheric air within their bodies.
Q93: Describe the function and location of the epiglottis.
Ans: The epiglottis is a thin, elastic cartilaginous flap located at the opening of the larynx. Its primary function is to cover the glottis during swallowing to prevent the entry of food into the larynx.
Q94: Describe the structural support system of the trachea and bronchi.
Ans: The trachea is a straight tube extending to the mid-thoracic cavity. The trachea, along with the primary, secondary, and tertiary bronchi, and the initial bronchioles, are supported by incomplete cartilaginous rings, which prevent them from collapsing.
Q95: Distinguish between the ‘conducting part’ and the ‘exchange part’ of the respiratory system.
Ans: The conducting part (from nostrils to terminal bronchioles) transports atmospheric air to the alveoli, clears it of foreign particles, humidifies it, and brings it to body temperature. The exchange part (alveoli and their ducts) is the site of the actual diffusion of oxygen and carbon dioxide between the blood and atmospheric air.
Q96: Why is the anatomical setup of the thoracic chamber considered “air-tight” and why is this essential?
Ans: The thoracic chamber is formed by the vertebral column, sternum, ribs, and diaphragm, creating a closed, air-tight unit. This setup is essential because we cannot directly alter pulmonary volume; we must change the thoracic volume to effect changes in the pulmonary volume for breathing.
Q97: Explain the mechanism of inspiration with reference to the pressure gradient.
Ans: Inspiration is the process of drawing atmospheric air into the lungs. It occurs when the intra-pulmonary pressure (pressure within the lungs) is less than the atmospheric pressure, creating a negative pressure gradient that forces air from the outside into the lungs.
Q98: Describe the specific role of the diaphragm during the process of inspiration.
Ans: Inspiration is initiated by the contraction of the diaphragm, which becomes flat. This contraction increases the volume of the thoracic chamber in the antero-posterior axis, contributing to the decrease in intra-pulmonary pressure required for inhalation.
Q99: Differentiate between Tidal Volume (TV) and Residual Volume (RV).
Ans: Tidal Volume (TV) is the volume of air inspired or expired during normal respiration, approximately 500 mL. Residual Volume (RV) is the volume of air remaining in the lungs even after a forcible expiration, averaging between 1100 mL and 1200 mL.
Q100: Explain the concept of Expiratory Reserve Volume (ERV) and provide its average value.
Ans: Expiratory Reserve Volume (ERV) represents the additional volume of air that a person can expire through a forcible expiration. This volume averages between 1000 mL and 1100 mL.
Three Mark Question and Answer
Q1: Elucidate the metabolic necessity for the respiratory system in living organisms.
Ans: Living organisms require a continuous supply of oxygen to indirectly break down simple molecules like glucose, amino acids, and fatty acids to derive energy for various activities. Concurrently, carbon dioxide, which is a harmful by-product of these catabolic reactions, must be released. Therefore, the respiratory system is essential to facilitate this continuous exchange of oxygen from the atmosphere with the carbon dioxide produced by the cells,.
Q2: Compare the respiratory mechanisms of sponges with those of earthworms.
Ans:
- Sponges: These are lower invertebrates that lack specialized respiratory organs. They exchange oxygen and carbon dioxide by simple diffusion over their entire body surface,.
- Earthworms: They also lack specialized respiratory systems but utilize their moist cuticle for respiration.
- Key Difference: While both use body surfaces, earthworms rely specifically on the moist nature of their cuticle to facilitate gas exchange, whereas sponges rely on direct diffusion from the water flowing through them (External context: water canal system).
Q3: Discuss the variation in respiratory organs among arthropods.
Ans: Arthropods exhibit different respiratory mechanisms based on their habitat. Aquatic arthropods, such as crustaceans (e.g., prawns), typically utilise special vascularised structures called gills for branchial respiration. In contrast, terrestrial insects possess a complex network of tubes known as tracheal tubes to transport atmospheric air directly within the body.
Q4: Classify the respiratory organs used by the different classes of vertebrates.
Ans:
- Fishes: They primarily use gills for respiration.
- Reptiles, Birds, and Mammals: These groups respire through vascularised bags called lungs (pulmonary respiration),.
- Amphibians: They have a dual system; they can respire through lungs and also through their moist skin (cutaneous respiration).
Q5: “Mechanisms of breathing vary among different groups of animals.” Justify this statement with examples.
Ans: The mechanism of breathing depends mainly on the habitat and level of organisation of the animal. For instance, lower invertebrates like flatworms use simple diffusion. Aquatic animals like molluscs use gills to extract oxygen from water. Terrestrial forms require lungs or tracheal systems to process atmospheric air. This diversity proves that respiratory mechanisms are evolutionary adaptations to specific environments.
Q6: Explain the concept of Cutaneous Respiration with a specific example.
Ans: Cutaneous respiration is the process of gas exchange across the skin or outer integument of an organism rather than through gills or lungs. This requires the skin to be kept moist and vascularised. A prime example is the frog (Amphibian), which can respire through its moist skin, particularly when underwater or during hibernation.
Q7: Define Pulmonary Respiration and list the terrestrial groups that utilize it.
Ans: Pulmonary respiration is the exchange of gases utilizing specialized vascularised bags called lungs. It is the primary mode of respiration for terrestrial vertebrates. The groups that utilize this method include amphibians, reptiles, birds, and mammals,.
Q8: Why is Carbon Dioxide considered a waste product that must be eliminated?
Ans: Carbon dioxide is released during the catabolic reactions that break down nutrients like glucose to release energy. It is potentially harmful to cells if it accumulates because it can alter the pH of body fluids (making them acidic) and interfere with metabolic processes. Therefore, it must be continuously released out of the cells.
Q9: Differentiate between the respiratory medium for aquatic vs. terrestrial animals.
Ans: Aquatic animals, such as fishes and aquatic arthropods, utilize water as their respiratory medium and extract dissolved oxygen using gills. Terrestrial animals, such as mammals and insects, utilize atmospheric air as their medium and extract oxygen using lungs or tracheal tubes.
Q10: What is the primary function of the catabolic reactions mentioned in the introduction?
Ans: The primary function of catabolic reactions involving glucose, amino acids, and fatty acids is to derive energy required to perform various bodily activities. Oxygen is utilized to facilitate these breakdown processes.
Q11: Describe the passage of air through the upper respiratory tract up to the glottis.
Ans: Air enters through a pair of external nostrils located above the upper lips. It travels through the nasal passage into the nasal chamber. The nasal chamber opens into the pharynx, which is a common passage for food and air. From the pharynx, air passes through the glottis (the opening of the windpipe) in the larynx region.
Q12: Explain the structure and function of the Larynx.
Ans: The larynx is a cartilaginous box located at the anterior end of the trachea. Its primary function is sound production, for which it is commonly called the “sound box”. It also houses the glottis, which is the entry point for air into the trachea.
Q13: What is the Epiglottis and why is it crucial for survival?
Ans: The epiglottis is a thin, elastic cartilaginous flap. Its crucial function is to cover the glottis during the act of swallowing. This prevents food and drink from entering the larynx and trachea, which would otherwise cause choking or aspiration into the lungs.
Q14: Describe the anatomy of the Trachea and its division.
Ans: The trachea is a straight tube that extends downwards through the neck into the mid-thoracic cavity. It is supported by incomplete cartilaginous rings to prevent collapse. At the level of the 5th thoracic vertebra, the trachea divides into two branches: the right and left primary bronchi.
Q15: Detail the hierarchy of the bronchial tree within the lungs.
Ans: After the trachea divides into primary bronchi, each bronchus undergoes repeated divisions to form secondary and tertiary bronchi. These further divide into smaller tubes called bronchioles, which eventually end up in very thin terminal bronchioles.
Q16: What are alveoli and how are they structurally adapted for their function?
Ans: Alveoli are vascularised, bag-like structures that arise from the terminal bronchioles. They have very thin, irregular walls. This thinness and rich blood supply (vascularisation) make them perfectly adapted for the rapid diffusion of gases between the air and the blood.
Q17: Explain the role of cartilaginous rings in the human respiratory system.
Ans: Incomplete cartilaginous rings are found supporting the trachea, primary, secondary, and tertiary bronchi, and the initial bronchioles. Their function is to keep these airways open and prevent them from collapsing under the pressure changes that occur during breathing, ensuring continuous airflow.
Q18: “The pharynx is a region of crossover.” Explain.
Ans: The pharynx is described as a common passage for both food and air. Food enters from the mouth and air enters from the nasal chamber; both pass through the pharynx before diverting into the oesophagus (food pipe) and trachea (windpipe) respectively.
Q19: Identify the structures that constitute the “Lungs” in human anatomy.
Ans: The lungs are not hollow bags but are comprised of a dense branching network. This network includes the bronchi (primary, secondary, tertiary), the bronchioles (initial and terminal), and the millions of alveoli. All these structures held together form the lung tissue.
Q20: Where are the lungs located and what protects them?
Ans: The lungs are situated in the thoracic chamber. They are protected dorsally by the vertebral column, ventrally by the sternum, and laterally by the ribs. Additionally, they are covered by a double-layered membrane called the pleura.
Q21: Explain the structure and function of the Pleura.
Ans: The pleura is a double-layered membrane covering the lungs. The outer layer is in contact with the thoracic lining, while the inner layer contacts the lung surface. Between these layers is the pleural fluid, which acts as a lubricant to reduce friction on the lung surface during respiratory movements.
Q22: Differentiate between the ‘Conducting part’ and the ‘Respiratory part’ of the respiratory system.
Ans:
- Conducting Part: Extends from external nostrils to terminal bronchioles. It transports air, clears foreign particles, humidifies air, and regulates temperature,.
- Respiratory (Exchange) Part: Consists of alveoli and their ducts. It is the site of actual gas diffusion (O2 and CO2) between blood and atmospheric air.
Q23: Describe the boundaries of the Thoracic Chamber.
Ans: The thoracic chamber is an anatomically air-tight chamber. It is bounded:
- Dorsally: By the vertebral column.
- Ventrally: By the sternum.
- Laterally: By the ribs.
- Lower side: By the dome-shaped diaphragm.
Q24: Why is the “anatomical air-tight setup” of the thorax essential for breathing?
Ans: This setup is essential because humans possess no direct muscle mechanism to alter the volume of the lungs (pulmonary volume) directly. Instead, breathing relies on changing the volume of the thoracic cavity. Because the thorax is air-tight, any change in thoracic volume is immediately reflected as a change in pulmonary volume, driving airflow.
Q25: List the specific functions of the conducting part of the respiratory system.
Ans:
- Transport: It conveys atmospheric air to the alveoli.
- Filtration: It clears the air of foreign particles (dust, microbes).
- Conditioning: It humidifies the air and brings it to body temperature to prevent damage to the delicate alveolar tissue.
Q26: Enumerate the five main steps involved in Respiration.
Ans:
- Breathing/Pulmonary ventilation (Inflow of air/Outflow of alveolar air).
- Diffusion of gases (O2/CO2) across the alveolar membrane.
- Transport of gases by the blood.
- Diffusion of O2 and CO2 between blood and tissues.
- Utilisation of O2 by cells for catabolism and release of CO2.
Q27: Explain the relationship between Thoracic volume and Pulmonary volume.
Ans: Due to the adhesive force of the pleural fluid and the air-tight nature of the thoracic chamber, the lungs adhere to the chest wall. Consequently, any expansion or contraction of the thoracic cavity causes a corresponding expansion or contraction in the lung (pulmonary) cavity.
Q28: What is the diaphragm and what is its anatomical position?
Ans: The diaphragm is a muscular, dome-shaped structure that separates the thoracic cavity from the abdominal cavity. It forms the floor (lower side) of the thoracic chamber and plays a critical role in generating the pressure gradients required for breathing,.
Q29: Why does the conducting part terminate at the terminal bronchioles?
Ans: The terminal bronchioles represent the end of the purely “tubular” transport system. Beyond this point, the structures (alveoli and alveolar ducts) become thin-walled and vascularised enough to allow for gas exchange, thus marking the beginning of the respiratory/exchange part.
Q30: How does the text define the “Exchange Part” of the respiratory system?
Ans: The exchange part is defined as the alveoli and their ducts. Its specific physiological role is the actual diffusion of oxygen and carbon dioxide between the blood in the capillaries and the atmospheric air stored in the alveoli.
Q31: Explain the principle of pressure gradients in the mechanism of breathing.
Ans: The movement of air into and out of the lungs is driven by pressure differences between the lungs and the atmosphere. Air always moves from high pressure to low pressure. Inspiration occurs when intra-pulmonary pressure is negative (lower) relative to atmospheric pressure. Expiration occurs when intra-pulmonary pressure is positive (higher) relative to atmospheric pressure.
Q32: Describe the mechanism of Inspiration.
Ans: Inspiration is active. It begins with the contraction of the diaphragm, which flattens and increases thoracic volume in the antero-posterior axis. Simultaneously, external intercostal muscles contract, lifting the ribs and sternum, increasing volume in the dorso-ventral axis. This total increase in volume lowers intra-pulmonary pressure, sucking air into the lungs.
Q33: Describe the mechanism of Expiration.
Ans: Normal expiration is passive. The diaphragm and external intercostal muscles relax. The diaphragm returns to its dome shape and the sternum/ribs drop to their normal position. This reduces thoracic and pulmonary volume, causing intra-pulmonary pressure to rise above atmospheric pressure, expelling air.
Q34: Differentiate between the roles of the Diaphragm and Intercostal muscles in increasing thoracic volume.
Ans:
- Diaphragm: Its contraction increases the thoracic chamber’s volume in the antero-posterior axis (top to bottom lengthening).
- Intercostal Muscles: The contraction of external intercostals increases the volume in the dorso-ventral axis (front to back expansion) by lifting the ribs and sternum.
Q35: How is the intra-pulmonary pressure lowered during inspiration?
Ans: According to Boyle’s Law (implied), pressure is inversely proportional to volume. During inspiration, the contraction of respiratory muscles results in an overall increase in the thoracic volume. This causes a similar increase in pulmonary volume. As the pulmonary volume increases, the intra-pulmonary pressure decreases to a level less than atmospheric pressure.
Q36: Define Intra-pulmonary pressure.
Ans: Intra-pulmonary pressure is the pressure of the air within the lungs (specifically the alveoli). Changes in this pressure relative to the constant atmospheric pressure determine the direction of airflow during breathing.
Q37: “Inspiration is a negative pressure breathing mechanism.” Explain.
Ans: Inspiration is called negative pressure breathing because air is drawn into the lungs rather than being forced in. This occurs because the pressure inside the lungs (intra-pulmonary pressure) drops below the atmospheric pressure outside. This creates a vacuum or “negative” pressure gradient that pulls air in.
Q38: What initiates the process of Inspiration?
Ans: Inspiration is initiated specifically by the neural signal stimulating the contraction of the diaphragm. This muscle action is the primary trigger that starts the volume expansion of the thoracic cavity.
Q39: How does the sternum move during breathing?
Ans: During inspiration, the contraction of the external intercostal muscles lifts the sternum up and forward. During expiration, the relaxation of these muscles allows the sternum to return to its original, lower position.
Q40: Can humans alter the strength of breathing? If so, how?
Ans: Yes, humans have the ability to increase the strength of both inspiration and expiration. This is achieved by utilizing additional muscles, specifically those in the abdomen, which can forcibly compress the thoracic cavity (for expiration) or assist in expansion.
Q41: What is a Spirometer and what is its clinical significance?
Ans: A spirometer is a device used to estimate the volume of air involved in breathing movements. Its clinical significance lies in the assessment of pulmonary functions; it helps diagnose respiratory conditions like asthma or fibrosis by measuring how much air a person can inhale/exhale and how quickly.
Q42: Define Tidal Volume (TV) and calculate the volume of air handled in one hour.
Ans: Tidal Volume is the volume of air inspired or expired during normal respiration, approx 500 mL. Calculation: Breathing rate is 12-16 times/min. Minute Volume = 500 mL x 12 = 6000 mL (min) to 8000 mL. Hourly Volume = 6000 x 60 = 360,000 mL to 480,000 mL (360-480 Liters). (External context: math based on).
Q43: Explain Inspiratory Reserve Volume (IRV) with values.
Ans: IRV is the additional volume of air a person can inspire by a forcible inspiration after a normal tidal inspiration. It represents the lung’s safety margin for deeper breathing. The average value is 2500 mL to 3000 mL.
Q44: Explain Expiratory Reserve Volume (ERV) with values.
Ans: ERV is the additional volume of air a person can expire by a forcible expiration after a normal tidal expiration. It represents the extra air that can be pushed out. The average value is 1000 mL to 1100 mL.
Q45: Define Residual Volume (RV) and explain why it cannot be measured by a standard spirometer.
Ans: RV is the volume of air remaining in the lungs even after a forcible expiration (approx. 1100-1200 mL). It prevents lung collapse. Since a spirometer only measures air that moves in or out of the mouth, and RV never leaves the lungs, it cannot be measured directly by this device.
Q46: Compare the volumes of ERV and RV.
Ans:
- ERV: The volume that can be forcibly exhaled (1000-1100 mL).
- RV: The volume that cannot be exhaled (1100-1200 mL).
- Comparison: They are similar in volume, but RV is slightly larger and represents the non-exchangeable “dead space” that keeps alveoli open.
Q47: Differentiate between Normal and Forcible Respiration in terms of volumes.
Ans: Normal respiration involves the Tidal Volume (TV) of ~500 mL. Forcible respiration involves the reserve volumes: Inspiratory Reserve Volume (IRV) for deep inhalation (2500-3000 mL) and Expiratory Reserve Volume (ERV) for deep exhalation (1000-1100 mL).
Q48: Provide the average breathing rate and explain how it relates to Minute Ventilation.
Ans: A healthy human breathes 12–16 times per minute. Minute ventilation is the total volume of air inhaled per minute. It is calculated by multiplying the Tidal Volume (500 mL) by the breathing rate, resulting in 6000–8000 mL of air per minute.
Q49: Why is Residual Volume important for gas exchange?
Ans: (Inference based on and text logic) Residual Volume ensures that there is always air in the alveoli. This allows for the continuous diffusion of O2 and CO2 between the blood and alveoli even during the pause between breaths or during expiration, preventing the blood passing the lungs from becoming deoxygenated.
Q50: Arrange the respiratory volumes (TV, IRV, ERV, RV) in descending order of magnitude.
Ans:
- IRV: 2500–3000 mL.
- RV: 1100–1200 mL.
- ERV: 1000–1100 mL.
- TV: ~500 mL.
Q51: Define Vital Capacity (VC) and explain its components.
Ans: Vital Capacity is the maximum volume of air a person can breathe in after a forced expiration (or breathe out after forced inspiration). It represents the maximum functional range of the lungs. Formula: VC = Expiratory Reserve Volume (ERV) + Tidal Volume (TV) + Inspiratory Reserve Volume (IRV).
Q52: Distinguish between Inspiratory Capacity (IC) and Expiratory Capacity (EC).
Ans:
- IC: The total volume a person can inspire after a normal expiration. Formula: TV + IRV.
- EC: The total volume a person can expire after a normal inspiration. Formula: TV + ERV.
Q53: What is Total Lung Capacity (TLC) and how is it calculated?
Ans: Total Lung Capacity is the total volume of air accommodated in the lungs at the end of a forced inspiration. It represents the absolute limit of lung volume. Calculation: TLC = Vital Capacity (VC) + Residual Volume (RV) OR TLC = RV + ERV + TV + IRV.
Q54: Explain Functional Residual Capacity (FRC).
Ans: FRC is the volume of air that remains in the lungs after a normal (tidal) expiration. This is the baseline air volume in the lungs during relaxed breathing. Formula: FRC = Expiratory Reserve Volume (ERV) + Residual Volume (RV).
Q55: Analyze the partial pressure gradients of Oxygen as per the provided data.
Ans:
- Alveoli: pO2 is 104 mm Hg.
- Blood (Deoxygenated): pO2 is 40 mm Hg.
- Blood (Oxygenated): pO2 is 95 mm Hg.
- Tissues: pO2 is 40 mm Hg.
- Analysis: Oxygen moves from Alveoli (104) -> Blood (40 becoming 95) -> Tissues (40) down its gradient.
Q56: Analyze the partial pressure gradients of Carbon Dioxide as per the provided data.
Ans:
- Tissues: pCO2 is 45 mm Hg.
- Blood (Oxygenated): pCO2 is 40 mm Hg.
- Blood (Deoxygenated): pCO2 is 45 mm Hg.
- Alveoli: pCO2 is 40 mm Hg.
- Analysis: CO2 moves from Tissues (45) -> Blood -> Alveoli (40) down its gradient.
Q57: Explain the significance of solubility in gas diffusion.
Ans: Solubility is a key factor affecting diffusion rates. The solubility of CO2 is 20-25 times higher than that of O2. This means that even with a much smaller partial pressure difference (gradient), CO2 can diffuse across the membrane much faster and more efficiently than O2.
Q58: Define Partial Pressure and state the values for O2 and CO2 in atmospheric air.
Ans: Partial pressure is the pressure contributed by an individual gas in a mixture of gases.
- Atmospheric Air pO2: 159 mm Hg.
- Atmospheric Air pCO2: 0.3 mm Hg.
Q59: Why does the pO2 drop from 159 mm Hg in the atmosphere to 104 mm Hg in the alveoli?
Ans: (Conceptual inference based on table data and respiratory biology): While atmospheric air has a pO2 of 159, alveolar air has a pO2 of 104. This drop occurs because the fresh air mixes with the “stale” air (Functional Residual Capacity) already in the lungs which has higher CO2 and water vapor, diluting the oxygen concentration.
Q60: Describe the direction of the concentration gradient for Oxygen and Carbon Dioxide.
Ans:
- Oxygen: Gradient is from Alveoli -> Blood -> Tissues.
- Carbon Dioxide: Gradient is in the opposite direction, from Tissues -> Blood -> Alveoli. This ensures O2 enters cells and CO2 leaves them.
Q61: Describe the structure and thickness of the Diffusion Membrane.
Ans: The diffusion membrane constitutes the barrier between the lung air and blood. It consists of three layers:
- Thin squamous epithelium of alveoli.
- Endothelium of alveolar capillaries.
- The basement substance between them. Despite these layers, the total thickness is much less than a millimetre.
Q62: How is Oxygen transported in the blood? Give percentages.
Ans: Blood transports oxygen in two forms:
- Bound to Haemoglobin: About 97% of O2 is transported by Red Blood Cells (RBCs) as oxyhaemoglobin.
- Dissolved in Plasma: The remaining 3% of O2 is carried in a dissolved state through the plasma.
Q63: How is Carbon Dioxide transported in the blood? Give percentages.
Ans: CO2 is transported in three forms:
- As Bicarbonate: Nearly 70% (major form).
- Bound to Haemoglobin: 20–25% (as carbamino-haemoglobin).
- Dissolved in Plasma: About 7%.
Q64: Explain the chemical interaction between Oxygen and Haemoglobin.
Ans: Haemoglobin is a red-coloured, iron-containing pigment in RBCs. Oxygen binds to haemoglobin in a reversible manner to form oxyhaemoglobin. Each haemoglobin molecule has 4 subunits and can carry a maximum of four molecules of O2.
Q65: Describe the Oxygen Dissociation Curve and its utility.
Ans: The Oxygen Dissociation Curve is a graph plotting the percentage saturation of haemoglobin with O2 against the partial pressure of oxygen (pO2). It typically results in a sigmoid (S-shaped) curve. It is highly useful for studying how factors like pCO2, H+ concentration, and temperature affect the binding of O2 to haemoglobin.
Q66: What conditions in the alveoli favor the formation of Oxyhaemoglobin?
Ans: The conditions in the alveoli are optimal for oxygen loading:
- High pO2.
- Low pCO2.
- Lesser H+ concentration (higher pH).
- Lower temperature.
Q67: What conditions in the tissues favor the dissociation of Oxygen from Haemoglobin?
Ans: The conditions in metabolically active tissues favor oxygen unloading:
- Low pO2.
- High pCO2.
- High H+ concentration (lower pH).
- Higher temperature.
Q68: “Haemoglobin acts as an efficient oxygen courier.” Justify.
Ans: Haemoglobin binds O2 in the lungs where pO2 is high and releases it in the tissues where pO2 is low. This reversibility makes it efficient. Under normal physiological conditions, every 100 ml of oxygenated blood delivers around 5 ml of O2 to the tissues.
Q69: Explain the effect of pCO2 on Oxygen binding (Bohr Effect context).
Ans: The text states that partial pressure of CO2 is a factor that can interfere with O2 binding. High pCO2 (as found in tissues) promotes the dissociation of oxygen from haemoglobin, while low pCO2 (as found in alveoli) promotes binding. This physiological phenomenon ensures O2 is delivered exactly where it is needed.
Q70: Why is the basement substance mentioned as a layer of the diffusion membrane?
Ans: The basement substance acts as the “glue” or structural matrix between the alveolar epithelium and the capillary endothelium. It comprises the thin basement membrane supporting the epithelium and the membrane surrounding the capillary cells. It is essential for structural integrity while remaining thin enough to permit rapid diffusion.
Q71: Explain the transport of CO2 as Carbamino-haemoglobin.
Ans: About 20-25% of CO2 is carried by haemoglobin as carbamino-haemoglobin. This binding is reversible and primarily related to pCO2. When pCO2 is high and pO2 is low (tissues), binding occurs. When pCO2 is low and pO2 is high (alveoli), dissociation occurs, releasing CO2,.
Q72: Describe the role of Carbonic Anhydrase in CO2 transport.
Ans: Carbonic anhydrase is an enzyme present in high concentration in RBCs (and trace amounts in plasma). It catalyzes the hydration of CO2 to form Carbonic Acid (H2CO3), which immediately dissociates into Bicarbonate (HCO3-) and Hydrogen ions (H+). This allows the majority of CO2 to be transported as bicarbonate.
Q73: Write the enzymatic reaction for CO2 transport catalyzed by Carbonic Anhydrase.
Ans: $$CO_2 + H_2O \rightleftharpoons H_2CO_3 \rightleftharpoons HCO_3^- + H^+$$ This reaction is reversible, facilitating CO2 trapping at tissues and CO2 release at alveoli.
Q74: Compare the chemical events occurring at the Tissue site vs. Alveolar site regarding CO2.
Ans:
- Tissue Site: Catabolism produces high CO2. CO2 diffuses into blood, reacts with water via Carbonic Anhydrase to form HCO3- and H+. CO2 is trapped as bicarbonate.
- Alveolar Site: pCO2 is low. The reaction proceeds in reverse. HCO3- and H+ combine to form H2CO3, which converts back to CO2 and H2O. CO2 is released.
Q75: “Every 100 ml of deoxygenated blood delivers approximately 4 ml of CO2 to the alveoli.” Derive the significance of this statement.
Ans: This statistic highlights the efficiency of the CO2 removal system. While blood carries a large load of CO2 (mostly as bicarbonate), a specific fraction (4ml/100ml) is unloaded at the lungs with every cycle to maintain the acid-base balance and remove waste products generated by metabolism.
Q76: Explain the Neural Regulation of Respiration.
Ans: Respiration is regulated by the neural system in the brain stem:
- Respiratory Rhythm Centre: Located in the medulla, primarily responsible for the basic rhythm.
- Pneumotaxic Centre: Located in the pons, moderates the rhythm centre to alter respiratory rate (usually by shortening inspiration).
Q77: Describe the Chemosensitive Regulation of Respiration.
Ans: A chemosensitive area adjacent to the rhythm centre in the medulla is highly sensitive to CO2 and Hydrogen ions (H+). An increase in these substances activates this centre, which signals the rhythm centre to increase the rate of breathing to eliminate CO2 and reduce H+ concentration.
Q78: What is the role of peripheral receptors in respiratory control?
Ans: Receptors associated with the aortic arch and carotid artery can recognize changes in CO2 and H+ concentration in the blood. Upon detecting increased levels, they send necessary signals to the respiratory rhythm centre for remedial actions (increasing breathing).
Q79: “The role of oxygen in the regulation of respiratory rhythm is quite insignificant.” Explain.
Ans: This statement implies that the respiratory control system is driven primarily by the need to remove CO2 and maintain pH (H+ levels), rather than a lack of Oxygen. The body is much more sensitive to CO2 buildup than it is to a drop in oxygen levels.
Q80: What is the Pneumotaxic centre and how does it alter the respiratory rate?
Ans: The Pneumotaxic centre is a neural centre in the Pons region. Its neural signal reduces the duration of inspiration. By shortening the time taken for a breath in, it effectively increases the number of breaths taken per minute (respiratory rate).
Q81: Distinguish between Asthma and Emphysema.
Ans:
- Asthma: An inflammatory disorder of the bronchi and bronchioles causing wheezing and difficulty in breathing. It is often allergic.
- Emphysema: A chronic disorder where alveolar walls are damaged, reducing the respiratory surface area. It is degenerative and strongly linked to cigarette smoking.
Q82: Describe Occupational Respiratory Disorders and their causes.
Ans: These are lung conditions caused by exposure to harmful substances in the workplace. In industries like grinding or stone-breaking, excessive dust is produced that overwhelms the body’s defense mechanisms. Long-term exposure leads to inflammation and fibrosis (proliferation of fibrous tissues), causing serious lung damage.
Q83: What is Fibrosis and in what context is it mentioned?
Ans: Fibrosis refers to the proliferation of fibrous tissues. It is mentioned in the context of Occupational Respiratory Disorders (like Silicosis/Asbestosis – implied). Inhaled dust particles cause chronic inflammation, leading to scar tissue formation (fibrosis) in the lungs, which reduces elasticity and gas exchange capability.
Q84: Based on the summary, how does the body transport the majority of Carbon Dioxide?
Ans: The summary reiterates that nearly 70 per cent of carbon dioxide is transported as bicarbonate (HCO3-). This process is facilitated by the enzyme carbonic anhydrase found in Red Blood Cells.
Q85: (From Exercises) Define Vital Capacity and explain its significance.
Ans: Vital Capacity is the maximum volume of air a person can breathe in after a forced expiration (ERV + TV + IRV). Its significance is that it represents the functional capacity of the lungs; a higher VC indicates better lung health and stamina, whereas a low VC can indicate restrictive lung diseases.
Q86: (From Exercises) What is Hypoxia? (External Source/General Knowledge as prompted by text).
Ans: Hypoxia is a condition characterized by a deficiency in the amount of oxygen reaching the tissues. It can be caused by low atmospheric oxygen (high altitude), lung issues (emphysema), or blood issues (anemia). It leads to dizziness, shortness of breath, and eventually cell death if untreated.
Q87: (From Exercises) What happens to the respiratory process in a man going up a hill?
Ans: As a man goes up a hill (altitude increases), the atmospheric pressure and partial pressure of oxygen (pO2) decrease. To compensate for the lower oxygen availability, the body increases the breathing rate and heart rate. Over time, acclimatization occurs, including increased RBC production (polycythemia).
Q88: Explain the significance of the Sigmoid pattern of the Oxygen Dissociation Curve.
Ans: The sigmoid (S-shape) pattern allows for two critical physiological functions:
- Plateau at high pO2: Ensures hemoglobin is almost fully saturated in the lungs even if atmospheric oxygen drops slightly.
- Steep slope at lower pO2: Ensures that small drops in tissue pO2 release massive amounts of Oxygen where it is needed most.
Q89: Why are workers in stone-breaking industries advised to wear masks?
Ans: Stone-breaking produces fine dust (silica). The body’s natural defenses (mucus/cilia) cannot cope with this high load. Inhaling this dust leads to inflammation and fibrosis. Masks filter out these particles, preventing the development of severe occupational respiratory disorders.
Q90: Summarize the role of the medulla oblongata in respiration.
Ans: The medulla oblongata houses the Respiratory Rhythm Centre and the Chemosensitive Area. The Rhythm Centre sets the basal breathing rate. The Chemosensitive area monitors CO2 and H+ levels in the blood and signals the Rhythm Centre to adjust breathing to maintain homeostasis.
Five Mark Question and Answer
Q1: Discuss the diversity of respiratory organs in the animal kingdom. How does the habitat and level of organisation influence the choice of respiratory mechanism?
Ans: The mechanism of breathing varies significantly among different animal groups, primarily driven by their habitats and levels of organisation.
- Simple Diffusion: Lower invertebrates like sponges, coelenterates, and flatworms generally lack specialized organs. They exchange Oxygen (O2) and Carbon dioxide (CO2) by simple diffusion over their entire body surface.
- Cutaneous Respiration: Earthworms use their moist cuticle for gas exchange. Amphibians like frogs also respire through their moist skin, known as cutaneous respiration.
- Tracheal System: Terrestrial insects utilize a network of tubes called tracheal tubes to transport atmospheric air directly within the body.
- Branchial Respiration: Aquatic arthropods (like prawns) and molluscs typically use vascularised structures called gills to respire in water.
- Pulmonary Respiration: Terrestrial vertebrates, including reptiles, birds, mammals, and adult amphibians, utilize vascularised bags called lungs for gas exchange.
Q2: Explain the metabolic necessity of respiration. Why must Oxygen be continuously provided and Carbon Dioxide released?
Ans:
- Metabolic Requirement: Organisms utilize Oxygen to indirectly break down simple nutrient molecules such as glucose, amino acids, and fatty acids. This catabolic process is essential to derive energy required to perform various bodily activities.
- Production of Waste: During these catabolic reactions, Carbon dioxide (CO2) is produced. Unlike useful by-products, CO2 is harmful to the cells if allowed to accumulate.
- The Exchange Process: Consequently, there is a dual necessity: Oxygen must be continuously provided to the cells to sustain energy production, and the CO2 produced must be released out. This process of exchange between atmospheric O2 and cellular CO2 is defined as breathing or respiration.
- External Context (Physiological pH): Accumulation of CO2 leads to the formation of carbonic acid, lowering blood pH (acidosis), which can be fatal. This emphasizes the need for efficient removal.
Q3: Describe the anatomy of the human upper respiratory tract from the external nostrils to the larynx. Include the functions of the epiglottis and larynx.
Ans:
- Nostrils and Nasal Chamber: Humans have a pair of external nostrils opening above the upper lips. These lead to a nasal chamber through the nasal passage.
- Pharynx: The nasal chamber opens into the pharynx. The pharynx is a critical region as it serves as the common passage for both food and air.
- Larynx (Sound Box): The pharynx opens through the larynx region into the trachea. The larynx is a cartilaginous box responsible for sound production, hence it is termed the “sound box”.
- Epiglottis: During the act of swallowing, the glottis (opening of the larynx) is covered by a thin, elastic cartilaginous flap called the epiglottis. This structure is vital as it prevents the entry of food into the larynx, which would otherwise obstruct the airway.
Q4: Detail the structure of the bronchial tree. What distinguishes the trachea and primary bronchi from the terminal bronchioles in terms of structural support?
Ans:
- Trachea: The trachea is a straight tube extending to the mid-thoracic cavity. At the level of the 5th thoracic vertebra, it divides into a right and left primary bronchus.
- Bronchial Divisions: Each primary bronchus undergoes repeated divisions to form secondary and tertiary bronchi. These further divide into smaller tubes called bronchioles, finally ending in very thin terminal bronchioles.
- Structural Support: The trachea, primary, secondary, and tertiary bronchi, as well as the initial bronchioles, are supported by incomplete cartilaginous rings. These rings prevent the collapse of the airway during breathing.
- Alveoli: The terminal bronchioles give rise to a number of very thin, irregular-walled, and vascularised bag-like structures called alveoli, which are the sites of gas exchange.
Q5: Differentiate between the ‘Conducting part’ and the ‘Exchange part’ of the respiratory system. What are the specific functions of the Conducting part?
Ans:
- Conducting Part: This includes the entire pathway starting from the external nostrils up to the terminal bronchioles. Its functions are:
- Transports atmospheric air to the alveoli.
- Clears the air of foreign particles.
- Humidifies the air.
- Brings the air to body temperature.
- Exchange (Respiratory) Part: This consists of the alveoli and their ducts.
- Function: It is the site of actual diffusion of O2 and CO2 between the blood and atmospheric air.
- Connection: The conducting part prepares the air, while the exchange part utilizes it for physiological gas exchange.
Q6: “The thoracic chamber is an anatomically air-tight chamber.” Explain the anatomical boundaries of this chamber and why this setup is essential for the mechanism of breathing.
Ans:
- Anatomical Boundaries: The thoracic chamber is formed:
- Dorsally: By the vertebral column.
- Ventrally: By the sternum.
- Laterally: By the ribs.
- Lower side: By the dome-shaped diaphragm.
- Mechanism: The lungs are situated inside this chamber. The anatomical setup is such that any change in the volume of the thoracic cavity is immediately reflected in the lung (pulmonary) cavity.
- Significance: This arrangement is essential because humans cannot directly alter the pulmonary volume (we have no muscles attached directly to the lungs to pull them open). We rely on changing the thoracic volume to generate the pressure gradients required for breathing.
Q7: Describe the mechanism of Inspiration. Explain the role of the diaphragm and intercostal muscles in generating the necessary pressure gradient.
Ans:
- Principle: Inspiration occurs when the intra-pulmonary pressure (pressure within the lungs) is less than the atmospheric pressure (negative pressure).
- Diaphragm Action: Inspiration is initiated by the contraction of the diaphragm. This flattens the diaphragm and increases the volume of the thoracic chamber in the antero-posterior axis.
- Intercostal Action: The contraction of external inter-costal muscles lifts the ribs and the sternum. This causes an increase in the volume of the thoracic chamber in the dorso-ventral axis.
- Result: The overall increase in thoracic volume causes a similar increase in pulmonary volume. This increase in volume decreases the intra-pulmonary pressure to below atmospheric levels, forcing air from the outside to move into the lungs.
Q8: Describe the mechanism of Expiration. How does the thorax return to its resting state and what happens to the intra-pulmonary pressure?
Ans:
- Principle: Expiration takes place when the intra-pulmonary pressure is higher than the atmospheric pressure.
- Relaxation: It is largely a passive process involving the relaxation of the diaphragm and the inter-costal muscles.
- Movement: Upon relaxation, the diaphragm returns to its original dome shape, and the sternum/ribs return to their normal positions.
- Volume and Pressure Change: This relaxation reduces the thoracic volume and thereby the pulmonary volume. This reduction in volume leads to an increase in intra-pulmonary pressure to slightly above the atmospheric pressure.
- Result: The higher internal pressure causes the expulsion of air from the lungs.
Q9: Define the following Respiratory Volumes and provide their average values: Tidal Volume (TV), Inspiratory Reserve Volume (IRV), and Expiratory Reserve Volume (ERV).
Ans:
- Tidal Volume (TV): The volume of air inspired or expired during a normal respiration. It is approximately 500 mL.
- Inspiratory Reserve Volume (IRV): The additional volume of air a person can inspire by a forcible inspiration. This averages 2500 mL to 3000 mL.
- Expiratory Reserve Volume (ERV): The additional volume of air a person can expire by a forcible expiration. This averages 1000 mL to 1100 mL.
- Clinical Relevance: These volumes can be measured using a spirometer to assess pulmonary function.
Q10: What is Residual Volume (RV)? Why does it exist, and how does it differ from the Expiratory Reserve Volume (ERV)?
Ans:
- Definition: Residual Volume (RV) is the volume of air remaining in the lungs even after a forcible expiration. It averages 1100 mL to 1200 mL.
- Existence: It exists to prevent the lungs from collapsing (atelectasis) and ensures that gas exchange can continue continuously between breaths.
- Difference from ERV:
- ERV (1000-1100 mL) represents the air that can be voluntarily expelled after a normal breath.
- RV represents the air that cannot be expelled voluntarily.
- Consequently, ERV contributes to Vital Capacity, whereas RV is only part of the Total Lung Capacity but not the Vital Capacity.
Q11: Define Vital Capacity (VC) and Total Lung Capacity (TLC). List the respiratory volumes that constitute each.
Ans:
- Vital Capacity (VC):
- Definition: The maximum volume of air a person can breathe in after a forced expiration (or breathe out after a forced inspiration).
- Constituents: VC = Expiratory Reserve Volume (ERV) + Tidal Volume (TV) + Inspiratory Reserve Volume (IRV).
- Total Lung Capacity (TLC):
- Definition: The total volume of air accommodated in the lungs at the end of a forced inspiration.
- Constituents: TLC = Vital Capacity (VC) + Residual Volume (RV) OR TLC = RV + ERV + TV + IRV.
- Significance: VC represents the functional range of breathing, while TLC represents the absolute anatomical limit.
Q12: Explain the physical basis of gas exchange in the alveoli. What are the three main factors that affect the rate of diffusion?
Ans:
- Physical Basis: Gas exchange occurs by simple diffusion driven mainly by pressure or concentration gradients.
- Partial Pressure: The individual pressure contributed by a gas (like O2 or CO2) in a mixture determines the gradient. Gases move from areas of high partial pressure to low partial pressure.
- Factors Affecting Diffusion:
- Pressure Gradient: The difference in partial pressure between alveoli and blood.
- Solubility: The solubility of the gases affects diffusion rates. For example, CO2 is 20-25 times more soluble than O2, allowing it to diffuse faster per unit of pressure difference.
- Membrane Thickness: The thickness of the membranes involved in diffusion (alveolar epithelium, basement substance, capillary endothelium) affects the rate. A thinner membrane facilitates faster diffusion.
Q13: Describe the structure of the Diffusion Membrane. Despite having multiple layers, why is it efficient for gas exchange?
Ans:
- Structure: The diffusion membrane is the barrier between the alveolar air and the pulmonary blood. It consists of three major layers:
- The thin squamous epithelium of the alveoli.
- The endothelium of the alveolar capillaries.
- The basement substance located in between them (composed of the basement membrane supporting the epithelium and the membrane surrounding the capillary endothelium).
- Efficiency: Despite consisting of these three layers, the total thickness of the diffusion membrane is much less than a millimetre. This extreme thinness, combined with the large surface area of the alveoli, ensures that the conditions are highly favourable for the rapid diffusion of O2 from alveoli to tissues and CO2 from tissues to alveoli.
Q14: Explain the transport of Oxygen in the blood. Describe the Oxygen Dissociation Curve and the factors that favor the formation of Oxyhaemoglobin.
Ans:
- Transport Forms: About 97% of O2 is transported by RBCs as oxyhaemoglobin. The remaining 3% is dissolved in plasma.
- Haemoglobin Binding: Haemoglobin is an iron-containing pigment. Each molecule can carry four O2 molecules reversibly.
- Dissociation Curve: Plotting the percentage saturation of haemoglobin against pO2 yields a sigmoid curve called the Oxygen dissociation curve.
- Favorable Factors (Alveoli): The formation of oxyhaemoglobin is favored in the alveoli where:
- pO2 is high.
- pCO2 is low.
- H+ concentration is lower (higher pH).
- Temperature is lower.
Q15: How is Carbon Dioxide transported in the blood? Explain the role of Carbonic Anhydrase in this process.
Ans:
- Modes of Transport:
- As Bicarbonate: Nearly 70% (major mechanism).
- Carbamino-haemoglobin: About 20-25% bound to haemoglobin.
- Dissolved in Plasma: About 7%.
- Role of Carbonic Anhydrase: RBCs contain a high concentration of the enzyme carbonic anhydrase (traces in plasma).
- Reaction: It catalyzes the reaction: $CO_2 + H_2O \rightleftharpoons H_2CO_3 \rightleftharpoons HCO_3^- + H^+$.
- At Tissues: High pCO2 drives the reaction forward, trapping CO2 as bicarbonate (HCO3-).
- At Alveoli: Low pCO2 drives the reaction backward, converting bicarbonate back to CO2 and H2O for release.
Q16: Discuss the Neural Regulation of Respiration. Describe the roles of the Respiratory Rhythm Centre, Pneumotaxic Centre, and Chemosensitive Area.
Ans:
- Respiratory Rhythm Centre: Located in the medulla region of the brain. It is primarily responsible for maintaining the basic respiratory rhythm to suit body demands.
- Pneumotaxic Centre: Located in the pons region. It moderates the functions of the rhythm centre. Neural signals from here reduce the duration of inspiration, thereby altering (increasing) the respiratory rate.
- Chemosensitive Area: Located adjacent to the rhythm centre. It is highly sensitive to CO2 and Hydrogen ions (H+). An increase in these substances activates this area, which signals the rhythm centre to make adjustments to eliminate these substances.
- Peripheral Receptors: Receptors in the aortic arch and carotid artery also detect CO2/H+ changes and signal the rhythm centre. Note: Oxygen plays an insignificant role in this regulation.
Q17: Describe the following respiratory disorders: Asthma, Emphysema, and Occupational Respiratory Disorders. Mention causes where applicable.
Ans:
- Asthma:
- Description: A difficulty in breathing causing wheezing.
- Cause: Inflammation of the bronchi and bronchioles.
- Emphysema:
- Description: A chronic disorder where alveolar walls are damaged, leading to a decrease in the total respiratory surface area.
- Cause: Cigarette smoking is a major cause.
- Occupational Respiratory Disorders:
- Description: Disorders occurring in industries like grinding or stone-breaking where defense mechanisms cannot cope with the high dust load.
- Consequence: Long-term exposure leads to inflammation and fibrosis (proliferation of fibrous tissues), causing serious lung damage.
- Prevention: Workers should wear protective masks.
Q18: (Based on Chapter Summary) Summarize the complete process of respiration from breathing to cellular utilisation.
Ans: The process of respiration involves several coordinated steps:
- Breathing (Ventilation): Atmospheric air is drawn in (inspiration) and alveolar air is released (expiration) driven by pressure gradients created by the diaphragm and intercostal muscles.
- Diffusion: O2 and CO2 diffuse across the alveolar membrane based on partial pressure gradients, solubility, and membrane thickness.
- Transport: Blood transports gases. O2 is carried chiefly as oxyhaemoglobin. CO2 is carried chiefly as bicarbonate (via carbonic anhydrase) and carbamino-haemoglobin.
- Exchange at Tissues: O2 dissociates from haemoglobin at tissues (where pO2 is low and pCO2/H+ is high) and diffuses into cells. CO2 diffuses from cells into blood.
- Cellular Respiration: Cells utilise the oxygen for metabolism to produce energy and release CO2 as a byproduct.
Q19: Describe the mechanism of breathing in humans. Explain how pressure gradients and specific muscle movements facilitate Inspiration and Expiration.
Answer: Breathing involves two stages: inspiration (drawing air in) and expiration (releasing air out). The movement of air is driven by creating a pressure gradient between the lungs and the atmosphere.
1. Inspiration:
- Pressure Gradient: Inspiration occurs when the pressure within the lungs (intra-pulmonary pressure) is less than the atmospheric pressure, creating a “negative pressure” in the lungs.
- Muscle Action: This is initiated by the contraction of the diaphragm, which flattens and increases the volume of the thoracic chamber in the antero-posterior axis. Simultaneously, the external inter-costal muscles contract, lifting the ribs and sternum, which increases the thoracic chamber volume in the dorso-ventral axis.
- Result: The overall increase in thoracic volume leads to a similar increase in pulmonary volume. This increase in volume decreases the intra-pulmonary pressure to below atmospheric pressure, forcing air from the outside to move into the lungs,.
2. Expiration:
- Pressure Gradient: Expiration takes place when the intra-pulmonary pressure is higher than the atmospheric pressure.
- Muscle Action: This is generally a passive process involving the relaxation of the diaphragm and inter-costal muscles. The diaphragm returns to its dome shape, and the sternum drops to its normal position.
- Result: This relaxation reduces the thoracic volume and, consequently, the pulmonary volume. This decrease in volume leads to an increase in intra-pulmonary pressure to slightly above atmospheric pressure, causing the expulsion of air from the lungs.
Humans also have the ability to increase the strength of inspiration and expiration using additional muscles in the abdomen.
Q20: Explain the transport of Carbon Dioxide (CO2) in the human body. Detail the modes of transport and the specific role of the enzyme carbonic anhydrase.
Answer: Blood is the medium of transport for CO2. It is transported in three specific forms:
- Dissolved in Plasma: About 7 per cent of CO2 is carried in a dissolved state through the plasma.
- As Carbamino-haemoglobin: About 20–25 per cent of CO2 is carried by haemoglobin as carbamino-haemoglobin. This binding is related to the partial pressure of CO2 (pCO2). In tissues where pCO2 is high and pO2 is low, binding occurs; in alveoli where pCO2 is low and pO2 is high, dissociation occurs,.
- As Bicarbonate: Nearly 70 per cent of CO2 is transported as bicarbonate.
Role of Carbonic Anhydrase: Red Blood Cells (RBCs) contain a very high concentration of the enzyme carbonic anhydrase (minute quantities are also in plasma). This enzyme facilitates the following reversible reaction in both directions,: CO2 + H2O →H2CO3 → HCO3– + H+
- At the Tissue Site: Due to catabolism, the partial pressure CO2 is high. CO2 diffuses into the blood (RBCs and plasma) and reacts with water to form HCO3– (bicarbonate) and H+.
- At the Alveolar Site: The partial pressure of CO2 is low. Here, the reaction proceeds in the opposite direction, converting bicarbonate back into CO2 and H2O.
Thus, CO2 is trapped as bicarbonate at the tissue level, transported to the alveoli, and released out as CO2. Every 100 ml of deoxygenated blood delivers approximately 4 ml of CO2 to the alveoli.
NCERT TEXTBOOK SOLVED QUESTIONS WITH ANSWERS
1. Define vital capacity. What is its significance?
Answer: Vital capacity (VC) is the maximum volume of air that a person can breathe out forcefully after a maximum forced inspiration. It represents the greatest amount of air that can be exchanged during a single breath. Vital capacity is an important indicator of pulmonary health and respiratory efficiency. A higher vital capacity indicates better physical fitness and greater ability of the lungs to supply oxygen to the body.
2. State the volume of air remaining in the lungs after normal breathing.
Answer: The volume of air remaining in the lungs after normal expiration is called the functional residual capacity (FRC). It is the sum of expiratory reserve volume (ERV) and residual volume (RV). In an average adult, it is approximately 2100–2300 mL.
3. Why does diffusion of gases occur only in the alveolar region and not in other parts of the respiratory system?
Answer: Diffusion of gases occurs only in the alveolar region because alveoli provide ideal conditions for gas exchange. They have extremely thin, moist walls, a very large surface area, and are richly supplied with blood capillaries. Other parts of the respiratory tract lack these features and therefore do not permit efficient diffusion of respiratory gases.
4. What are the major transport mechanisms for carbon dioxide in blood? Explain.
Answer: Carbon dioxide is transported in blood by three main mechanisms. About 70% of CO₂ is transported as bicarbonate ions in the plasma. Approximately 20–25% of CO₂ binds with haemoglobin to form carbamino-haemoglobin. The remaining 7% of CO₂ is transported in dissolved form in the plasma. Transport of CO₂ depends on its partial pressure.
5. What will be the pO₂ and pCO₂ in atmospheric air compared to alveolar air?
Correct option: (ii) pO₂ higher, pCO₂ lesser
Answer: Atmospheric air has a higher partial pressure of oxygen and a lower partial pressure of carbon dioxide compared to alveolar air. In the alveoli, oxygen diffuses into the blood while carbon dioxide diffuses from the blood into the alveolar air, resulting in lower pO₂ and higher pCO₂ in alveolar air.
6. Explain the process of inspiration under normal conditions.
Answer: Inspiration is the process by which fresh air enters the lungs. It occurs due to contraction of the diaphragm and external intercostal muscles. The diaphragm flattens and the ribs move upward and outward, increasing the volume of the thoracic cavity. As a result, intrapulmonary pressure decreases below atmospheric pressure. Air then flows into the lungs due to the pressure difference.
7. How is respiration regulated in humans?
Answer: Respiration is regulated by both nervous and chemical mechanisms. The respiratory centres are located in the medulla oblongata and pons. The dorsal respiratory group primarily controls inspiration, while the ventral respiratory group regulates both inspiration and expiration. The pneumotaxic centre in the pons regulates the rate and depth of breathing. Chemically, respiration is regulated by chemoreceptors in the carotid and aortic bodies, which respond mainly to changes in carbon dioxide and hydrogen ion concentration in the blood.
8. What is the effect of pCO₂ on oxygen transport?
Answer: An increase in pCO₂ causes a rightward shift of the oxygen-haemoglobin dissociation curve, reducing the affinity of haemoglobin for oxygen. This phenomenon is known as the Bohr effect. It facilitates the release of oxygen from haemoglobin in the tissues where carbon dioxide concentration is high.
9. What happens to respiration in a person going up a hill?
Answer: At high altitudes, the partial pressure of oxygen decreases. As a result, the rate and depth of breathing increase to compensate for reduced oxygen availability and to maintain adequate oxygen supply to the tissues.
10. What is the site of gaseous exchange in insects?
Answer: In insects, gaseous exchange occurs through the tracheal system, specifically the tracheae and tracheoles.
11. Define oxygen dissociation curve. Why does it show a sigmoidal shape?
Answer: The oxygen dissociation curve is a graph showing the relationship between the partial pressure of oxygen (pO₂) and the percentage saturation of haemoglobin with oxygen. The curve is sigmoid in shape due to cooperative binding of oxygen to haemoglobin. At high pO₂, haemoglobin binds oxygen strongly, while at low pO₂, oxygen is released rapidly, producing the characteristic S-shaped curve.
12. What is hypoxia? Explain its types.
Answer: Hypoxia is a condition in which body tissues do not receive adequate oxygen.
- Hypoxic hypoxia occurs at high altitudes due to low oxygen availability.
- Anaemic hypoxia results from reduced oxygen-carrying capacity of blood due to anaemia or carbon monoxide poisoning.
Both conditions lead to reduced oxygen supply to tissues.
13. Distinguish between the following:
Answer: (a) IRV and ERV
| Feature | IRV (Inspiratory Reserve Volume) | ERV (Expiratory Reserve Volume) |
| Definition | Additional volume of air that can be forcibly inhaled after a normal inspiration | Additional volume of air that can be forcibly exhaled after a normal expiration |
| Nature | Inspiratory volume | Expiratory volume |
| Role | Helps increase oxygen intake during forceful breathing | Helps expel more air during forceful expiration |
Answer: (b) Inspiratory capacity and expiratory capacity
| Feature | Inspiratory Capacity (IC) | Expiratory Capacity (EC) |
| Definition | Maximum volume of air that can be inhaled after a normal expiration | Maximum volume of air that can be exhaled after a normal inspiration |
| Components | Tidal Volume + IRV | Tidal Volume + ERV |
| Function | Indicates inhalation efficiency | Indicates exhalation efficiency |
Answer: (c) Vital capacity and total lung capacity
| Feature | Vital Capacity (VC) | Total Lung Capacity (TLC) |
| Definition | Maximum volume of air that can be expelled after a forced inspiration | Total volume of air present in the lungs after a forced inspiration |
| Includes Residual Volume | No | Yes |
| Significance | Indicates pulmonary health | Represents total lung volume |
14. What is tidal volume? Find out the tidal volume (approximate value) for a healthy human in an hour.
Answer: Tidal volume is the volume of air inspired or expired during a normal, quiet breath. In a healthy adult, the tidal volume is approximately 500 mL per breath. Out of this, about 350 mL reaches the alveoli and participates in gas exchange, while about 150 mL remains in the dead space and does not take part in gas exchange.
A healthy adult breathes about 12–16 times per minute.
Therefore, air exchanged per minute = 500 mL × 12–16 = 6000–8000 mL (6–8 L)
Hence, tidal volume exchanged in one hour = 360–480 litres of air.
Questions and Answers Compiled by AKB SIr